
Introduction
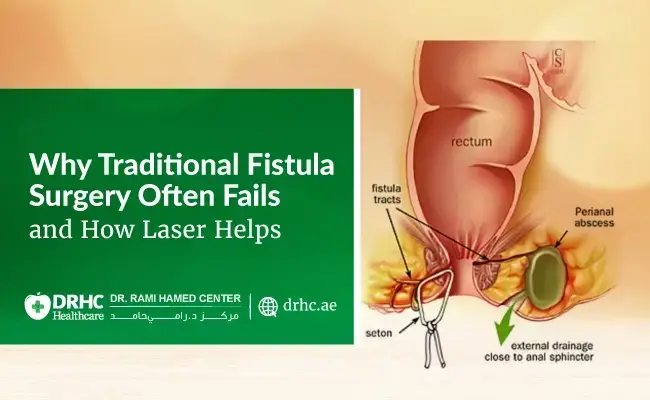
An anal fistula is a small granulation tissue tract. The tract joins a secondary entrance in the perianal skin (external orifice) to a primary opening within the anal canal in the lower part of the bowel (internal orifice).
Primary causes of anal fistulas include anorectal abscesses, fistulas from anal abscesses can occur anywhere between 15- 38% of the time, and a tiny tract may remain after the pus drains out.

Secondary causes include:
- Trauma
- Crohn's disease
- Tuberculosis
- Cancer
- Specific infections (HIV, chlamydia, actinomycosis)
- Radiation
- And anal fissures.
Generally, male: female ratio in anal fistulas is 2:1.
Anal fistula symptoms are including:
- Unpleasant discharge.
- Skin irritation, redness, itching
- Anal discomfort
Classification of anal fistula:

Anal fistulae are divided into four group according to Parks classification:
- Inter sphincteric fistula: The most common anal fistula, mainly limited in the intersphincteric plane
- Trans sphincteric fistula: Penetrates the external sphincter muscle.
- Supra sphincteric fistula: Penetrates the levator ani and passes above the external sphincter muscle
- Extra sphincteric fistula: Lies entirely outside of the sphincter apparatus, connecting the rectum to the perineal skin.
Clinically, anal fistula can also be divided into two groups: simple and complex.
- Simple anal fistula:
- Single Tract
- Fistula tract only penetrates up to 30–50% of external anal sphincter
- Complex Anal Fistula:
- Multiple tracts
- It penetrates more than 30-50% of external anal sphincter
- Mainly found in an anterior location at 12 o clock in lithotomy position
- Most likely caused by pelvic radiation or Crohn's disease.
MRI pelvic with contrast is generally used for initial diagnostic assessment and treatment plan management:
- Determination the type of
- Determination the primary fistula tract and its secondary
- Determination associated
- Detection of inflammatory tissues or
- For long-term outcomes assessment.
The treatment of anal fistula mainly is surgical intervention.
the surgical treatment options available for anal fistulae include both traditional and minimally invasive techniques.
The traditional surgical methods include:
- Fistulotomy (laying open of the tract): For low fistula.
- Fistulectomy (excision of the tract): For low fistula.
- Seton placement: For high and complex fistula.
- Local advancement flap: For high and complex fistula.
Traditional techniques have been associated with the incidence of incontinence especially in recurrent cases.
The minimally invasive methods include:
- Fibrin glue
- Bio-prosthetic plugs
- Ligation of intersphincteric fistula
- Anal fistula laser treatment FiLAC.
- Video assisted anal fistula treatment VAAFT.
VAAFT
Professor P. Meinero developed the Video-Assisted Anal Fistula Treatment VAAFT in 2006.
Using a specially made fistuloscope, VAAFT includes locating the internal fistula opening, securely closing internal orifice, and exploring all fistula tract before cauterizing and closing it from inside, and discover any additional tract/abscess along with fistula tract.
VAAFT is designed to affect the walls of fistula tract only, preserving sphincter muscle and avoiding fecal continence.
By doing this procedure under direct view, video assisted anal fistula treatment VAAFT avoids sphincter damage, which is its primary advantage over other procedures, while conventional methods such as fistulotomy, seton placement, fistulectomy, have side effects that included 4–5% soft stool incontinence, 30% flatus incontinence.
Wound in VAAFT is a quite minor and does not require wound packing.
There is a little pain during the recovery phase after procedure.
VAAFT surgery has a reported success rate of 70–80%.
This is an appropriate time for remembering our dear anal fistula patients that we have been entrusted with their care, we should treat them with the same respect as our own family, and should choose which method would we like to apply to them?
Indications of VAAFT procedure:
- Well-formed Fistula
- Recurrent Fistula
- Complex Fistula
- Multiple tract Fistula
Contraindications of VAAFT procedure:
- acute inflammation
- Low perianal
- Submucous
- Pelvic fistula
- systemic diseases (Crohn’s disease, tuberculosis, pelvic radiation).
VAAFT Equipment’s:

- High resolution scope with straight working channel and irrigation channel, this scope is going inside the fistula tract for video guidance anal fistula treatment.
- Tiny grasper (endoforceps)
- Endobrush for granulation tissues removal
- Volkmann Spoon for cleaning the tract
- Unipolar Electrode for fulguration of tract wall, it is connected to a high frequency generator
- Regular Anoscope
- Stitches or stapler
- irrigation
Essential features of VAAFT technique:
- Exploration of the fistula tract by fistuloscope.
- Localization of the internal fistula
- Exploration of secondary fistula tracts and abscess
- Destruction of the fistula tract walls under direct vision
- Securely closure of the internal fistula
VAAFT Procedure Steps:
- The procedure is usually performed in operation theatre under general
- The patient position is lithotomy position with head down 20 degree.
- Assembly of instruments:
- the fistuloscope is attached to the light source.
- the fistuloscope is connected to the irrigation tube, which is attached to an irrigation fluid.
- Examination of anus and perianal skin for identification of external fistula opening.
- Assessment of anorectal by proctoscopy for localization of internal fistula opening.
- Using the tip of a fistula probe, the external fistula opening is dilated.
- Excision of fibrous scar tissue, widening an external opening to create smooth entry of the fistuloscope.
- The fistuloscope tip is positioned slightly inside the external opening before the irrigation is started to expand and identify the fistula tract.
- The irrigation solution causes the fistula tract to expand, which allows fistuloscope gradually pushed through it.
- the fistuloscope is slowly advanced vertically, rotatorily, or side-to-side.
- The real-time image on the video monitor at the patient's head serves as the basis for guidance during the surgical steps.
- Granulation tissue in the form of white flakes are seen inside a fistula tract, which typically forms a fistula tunnel.
- At this point, a next step gets started to determine the internal fistula opening's location.
- To locate the internal opening's position, an anal retractor is inserted into anal canal.
- A jet of irrigating fluid is frequently seen coming from the internal opening through anal canal.
- The fistuloscope itself can passed into the anal canal through the internal opening in certain patients with a well-defined fistula tract and a big internal opening.
- In certain cases, the internal hole could be completely hidden by a mucosal fold, then the operation room lights are switched off, the transillumination effect of the fistuloscope's light beaming through the mucosal wall may help locating the internal opening.
- If the internal opening cannot be located, there is no need to try more attempts, it may make a fake internal opening.
- After the fistula's internal opening on the anal wall has been identified, it is isolated and marked with three long sutures.
- The full thickness of the rectal mucosa is stitched through.
- Sutures are positioned distally, at the opening, and proximally to the internal opening, respectively.
- An artery forceps is used to hold the long tails of the sutures outside of the anal canal.
- Following localization and isolation of the internal opening using sutures, the entire fistula tract is inspected for additional fistula tracts and small abscesses.
- Starting at the external opening, the fistuloscope is used to reexamine the whole fistula tract, the fistuloscope is advanced to look for additional fistulous tracts and hidden abscesses.
- Once an abscess cavity has been identified, drainage should be done followed by abscess wall fulguration.
- The fistuloscope is used to pass through any secondary tracts that may exist, and unhealthy tissues on the tract wall are fulgurated.
- The whole walls of the main fistula tract are fulgurated as well.
- A monopolar electrode that is passed through the fistuloscope's operating channel is used to carry out the fulguration process.
- Debridement is finished using an Endobrush that is passed via the fistuloscope operating channel and a Volkmann spoon after removal of the fistuloscope.
- Removed tissue is sent for histopathology.
- Returning the anal retractor at this step affords a clear view of the internal opening to close it properly by sutures or linear stapler.
- Hemostasis
- The external opening is covered with a dressing.
The pilonidal sinus can also be treated with this method, EPSiT (endoscopic pilonidal sinus treatment).
Topic: Proctology General Surgery



.jpg)

.webp)
.webp)

Leave a comment